
Both diabetes and periodontal diseases are common chronic diseases. This article describes the current evidence regarding the relationship between periodontal infections and glycemic control in diabetes. In some individuals, the pathogenesis of diabetes as well as the state of poorer glycemic control appears linked with inflammation and infection. There are important characteristics of periodontal infection that suggest a biologically plausible link to systemic inflammation and adverse effects on glycemic control. There is also empirical evidence that suggests treating periodontal infection can lead to improved glycemic control. There still remains sufficient variation in the body of literature to recommend additional, large-scale definitive studies. However, the implications of treating periodontal infection on glycemic control may have important potential in managing diabetes and in reducing the burden of diabetes.
This article describes the current evidence regarding the relationship between periodontal infections and glycemic control in diabetes. The epidemiologic data are based on the United States, but the patterns of association are nevertheless becoming increasingly common in other parts of the world. The focus is on oral health and diabetes in the United States, but it reflects the emerging epidemic of diabetes in various parts of the world. This article covers diabetes, periodontal diseases, and insulin resistance, as well as how they might be interrelated through epidemiologic studies and plausible biologic mechanisms. Additionally, this article considers observational and clinical studies pertaining to periodontal infection having an adverse effect on glycemic control.
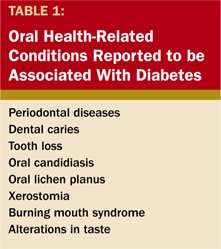
There is very strong and consistent evidence that diabetes has an adverse effect on periodontal health.1 Table 1 shows other oral health-related conditions which have been reported to be associated with diabetes but will not be considered in this discussion. The evidence is varied, but stronger evidence exists for the relationship between diabetes and periodontal diseases than for any of the other oral health-related conditions.
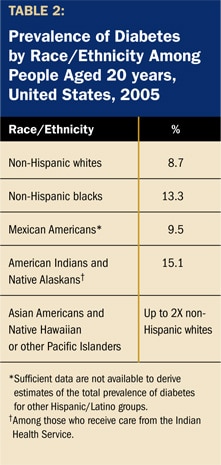
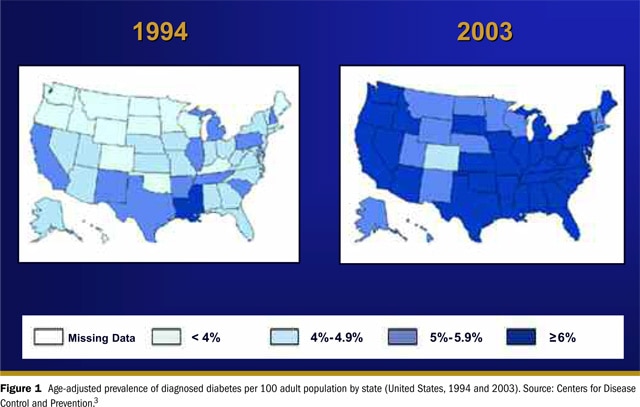
In the United States, diabetes is a very prevalent, common, chronic disease. Approximately 20.8 million people or 7% of the US population has diabetes,2 and 30%of the people with diabetes have not been diagnosed. In the United States, the prevalence of type 2 diabetes is associated with age and minority status. Among people >=60 years, the prevalence of diabetes is approximately 3 times greater than the prevalence for people of all ages.2 Table 2 shows the distribution of diabetes prevalence among US minority populations. Several minority ethnic populations are more likely to have diabetes than non-Hispanic white individuals of similar age in the United States.2
Burden of disease
Diabetes
Diabetes imparts a tremendous burden associated with its complications. These complications include heart disease and stroke, high blood pressure, visual impairment (leading to blindness), renal disease, nervous system disease, amputations, complications of pregnancy, and greater susceptibility to many other illnesses.2 The monetary burden has been reported as approximately $132 billion US dollars with $92 billion in direct medical costs and $40 billion in indirect costs (eg, disability, work loss, and premature mortality).2
Periodontal Disease
Periodontal disease is a chronic inflammatory disease of bacterial ideology. The importance of gram-negative pathogens becomes crucial in considering the relationships between periodontal disease and glycemic control. The local effects of the host response to periodontal infection include tissue destruction and, in severe cases, tooth loss.However, it is now believed that there may be additional systemic effects from periodontal disease.
Like diabetes, periodontal disease is a very common chronic disease among the US population. Across all ages, >50% of the US population has gingivitis. The prevalence of severe periodontitis (measuredby loss of periodontal attachment >=6 mm) increases with age. On average, approximately 13% of the population has moderate or severe periodontitis.4
Join us
Get resources, products and helpful information to give your patients a healthier future.
Join us
Get resources, products and helpful information to give your patients a healthier future.







